Neuropathy in Lombard, IL
The team at West Suburban Podiatry Associates believe that well-informed patients make better heath and life decisions. That is why we've included information below about many of the foot conditions we treat. Please take a look and contact us with any questions you may have.
Neuroma
(Perineural Fibroma)
What is it?
A neuroma is a painful lesion involving any nerve. In the foot the most common area is in between the third and fourth toes. The space in between the second and third toes is another commonly affected area. Neuromas are caused by trauma or damage to the nerve resulting in scaring and fibrosis. The damage may take years to accumulate and may be from fairly normal wear and tear. These are benign tumors with very little chance of malignancy.
What causes neuromas?
No one has isolated one single cause. It is most likely a combination of factors including: tight shoes, loose ligaments, shear within the nerve, and pressure from neighboring bone. Ill-fitting shoes or abnormal bone movement often instigate the pathological process.
Signs and Symptoms
- Burning
- Tingling
- Popping in the foot
- Cramping
- Electrical sensations
- Numbness
- Shooting pains
- Sensation of walking on a pebble
Treatment
Early treatment modalities include shoe gear changes, ice application, padding and strapping, arch supportive therapy, and cortisone injections. As time goes by the nerve can become deeply scarred and fibrosed to the surrounding structures. The damage eventually becomes irreversible. When early treatment is initiated there is a good chance of success. When the neuroma has been symptomatic for more than six months the effectiveness of conservative care drops and surgically removing the neuroma becomes a better option. The surgery is done under local anesthesia in an outpatient facility. The surgery removes the scar tissue and the damaged nerve leaving a numb area between the involved toes.
Gout
Gout can produce a form of arthritis that usually affects one joint, most commonly the first metatarsal-phanlangeal joint (the big toe joint). While the most common form affects men, especially after the age of 45, it may be seen infrequently in post-menopausal women. Gout is a metabolic disturbance that results from the over-production or under-secretion of uric acid. Uric acid comes from our intake of foods, which normally contain amino-acids called purines. Purines break down into uric acid. Different foods contain different amounts of purines. If the blood contains an excess of uric acid, there can be that tendency for it to crystallize within the joints, such as the big toe joint. This usually results in severe pain, redness, and swelling. Even vibrations in the room are enough to aggravate the pain in a classic attack. Fortunately, attacks can be treated with several medications and certain dietary changes. One medication is Indocin, which is a commonly dispensed anti-inflammatory. Other medications used to treat gout include Colchicine, Allopurinol, and Probenecid. Colchicine is a gout specific anti-inflammatory. Allopurinol and Probenecid can be used to control the underlying cause of having too much uric acid, either over-production or under-secretion, respectively.
Treatment of Gout by Diet
Foods Allowed in the Treatment of Gout (Low in Purine)
Cereals
(except whole grain)
Cream
Tapioca
Cucumber
Beet greens
Rutabaga
Breads
(except whole grain)
Egg
Butter and all fats
Eggplant
Broccoli
String beans
Potato
(white and sweet)
Fruit
Cabbage
Brussels sprouts
Pumpkin
Lettuce
Milk
Carrots
Celery
Turnip
Beets
Tomato
Foods Allowed Occasionally in the Treatment of Gout
Chicken
Fresh salmon
Haddock
Oyster
Bacon
Crab
Whitefish
Lobster
Lamb
Foods to Avoid in the Treatment of Gout (High in Purine)
Whole grain cereals
Beef
Codfish
Spinach
Mushrooms
Kidney beans
Turkey
Meat soup
Horseradish
Alcohol
Coffee
Whole grain bread
Veal
Brains
Watercress
Lima beans
Sausage
Squab
Kidney
Garlic
Catsup
Cocoa
Sweetbread
Goose
Calf's tongue
Radish
Navy beans
Anchovy
Bouillon
Sardine
Mustard
Pepper
Liver
Pike
Lentil
Peas
Perch
Pork
Gravy
Paprika
Spices
Tea
Plantar Fasciitis
Heel Spur Syndrome

What is the plantar fascia?
The plantar fascia is a strong thick band of connective tissue that runs along the bottom of the foot. It functions to help support the arch of the foot. The plantar fascia begins at the calcaneus (heel bone) and ends at the base of the toes.
This is a term that describes inflammation of the plantar fascia. There are several terms used to describe this condition including heel spur syndrome, plantar fasciitis, and heel pain syndrome. When inflamed, the plantar fascia tends to hurt in the heel and arch areas. With long term (chronic) fasciitis, the heel bone reacts by laying down minerals within the fascia at its insertion giving the appearance of a heel spur.
Symptoms of Plantar Fasciitis?
The most consistent finding with plantar fasciitis is post-static dyskinesia. This is pain after rising from a period of non-weight bearing, such as arising from bed in the morning or standing up after working at your desk for several hours. This pain will usually subside after a short while only to return later. Other common symptoms include arch pain, fullness/swelling in the heel, or the feeling of a bone bruise.
Causes of plantar fasciitis:
- Sudden increase in activity level without proper stretching
- Poor foot mechanics
- Pronation (foot rolls in/fallen arch)
- Structural foot problems
- Trauma/injury
- Standing/walking on hard surfaces
- Climbing ladders or stairs
- Poor shoes
- Flat feet
- High arch feet
- Weight gain
- Pushing objects
- Post-partum
Diagnosis
Onset:
Usually gradual with progression of symptoms. Patients average three to four months after initial onset before seeking medical attention.
Pain:
Deep ache on bottom of heel and arch pain. Especially painful when putting weight on the heel after periods of rest i.e. the first few steps.
X-rays:
Used to rule out bony abnormalities or fractures. Also helpful in visualizing tissue effusion, soft tissue swelling, and spurs.
Differential Diagnosis
- Stress fracture
- Bursitis
- Stone bruise
- Infection
- Nerve entrapment
- Arthritides
- Tendonitis
- Radiculopathy (low back)
Treatment of Plantar Fasciitis
The vast majority of patients with plantar fasciitis/heel spur syndrome improve dramatically with a course of good conservative care. The interval of time between initial onset of symptoms and beginning of therapy correlates directly with poor prognosis. In other words, the longer it takes to seek help, the longer it takes to reduce the inflammation and control the mechanics. However, it should be emphasized that conservative care is effective over 95% of the time. If conservative therapy fails, there are surgical options available. These surgeries are almost always done in an out-patient setting meaning you are able to walk in and out of the surgery center or hospital on the same day.
Conservative care
1. Control foot mechanics
The abnormal forces acting on the fascia must be controlled. If you eliminate/reduce the stress, you eliminate/reduce the cause of the inflammation. The two most effective methods are strapping (taping the foot) and orthotics (custom molded shoe inserts).
2. Anti-inflammatory modalities
The inflammation must be reduced as quickly as possible. The anti-inflammatory portion of the treatment regime is probably the least important, but it is the quickest to achieve its goal. Anti-inflammatory modalities include ice application, oral medication, and cortisone injections.
3. Physical therapy
Physical therapy is key to overcoming inflammation and decreasing the likelihood of reoccurrence. Physical therapy treatment modalities include stretching, ultrasound, iontophoresis, ice massage, and education.
Only after a full course of unsuccessful conservative therapy should surgery be considered. The goal of surgery is to functionally lengthen the plantar fascia. The procedure releases a portion of the plantar fascia near its insertion at the heel. This allows the fascia to heal in a lengthened fashion. As mentioned above, this procedure is usually performed in an out-patient setting, meaning no overnight hospital stay. Additionally, it should be noted that following the surgery you usually do not need crutches and are encouraged to walk utilizing a post-op stiff sole shoe.
Proper Fitting Shoes
TIPS ON HOW TO BUY PROPER FITTING SHOES
- Well constructed, proper fitting shoes are the key to a lifetime of pain-free walking.
- The most important factor in buying shoes is to pick a size and style that is appropriate for the activity you plan to use the shoe for. Athletic shoes are always the best for exercise or for working long hours on your feet.
- Do not plan to “break in” shoes. They should fit well all over your feet in the store.
- Shoes should have plenty of room for your toes. There should be at least a thumbs width from the longest toe to the end of the shoe while standing.
- Different brands and styles can run larger or smaller than your regular size so don't hesitate to try a size bigger or smaller to get the best fit.
- The sole of the shoe should be made of thick material to absorb shock and give support. There should be good built-in arch support. Thin leather soles give poor cushioning and poor support for your foot.
- Pick a shoe with a very stiff heel counter area. This will provide better support and function.
- Heels should be limited to less than 1 ½ inches.
- Some medical conditions or foot deformities require special fitting of shoes or specially made insoles. Contact our office at the number above if you have continued pain or other special conditions.
Hammertoes

An inherited muscle imbalance or abnormal bone size can make any number of toes buckle. The joints in time “contract” causing tendons to shorten. Corns or calluses can result from the deformity.
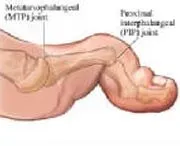
Hammertoes are either a flexible or rigid contracture of any of the smaller toes. One or any number may form on any one foot. Even the big toe can “contract” in some instances. This contracture typically occurs at the first toe joint (the one closest to your heel), however, it may occur at the more distal joint. In these circumstances, when the more distal joint is involved, the term “mallet toe” is more appropriate. If both joints are contracted, then the term “claw toe” is used. Hammertoes can also cause pain, corns, and calluses in-between the toes. This most commonly occurs, in-between the fourth and fifth toes.
Shoes, activities, and even arthritis in most cases are not necessarily the leading cause of this deformity. Typically, one's own inherited foot structure is the cause. This accounts for the strong family inheritance of this deformity. In some cases, having a “crooked toe” does not mean it may lead to a problem. However, unremitting sores, corns, and calluses can form in time. This can make the wearing of some shoes uncomfortable and difficult. Conservative care can be helpful but must be usually continued at routine intervals for what can be a lifetime.
Treatment should depend on many factors, such as: the patient's complaint, responsiveness to conservative care, patient's age, and other relevant medical history or problems. Conservative care may include doing nothing, staying out of tight fitting shoes, padding the toe, occasional trimming any build up of dead skin (corns and calluses), and the application of a pumice stone and moisturizing lotion at home. Additionally, shoe gear modifications can be helpful as well as arch supports or orthotics. When conservative care fails to provide relief, surgery may be indicated.
Surgical correction typically involves one or both of two major types of corrections: soft-tissue and bony. Soft tissue correction is usually indicated for any “flexible” deformity. Soft tissue correction involves releasing ligaments and tendons. Bony correction is indicated for any “rigid” deformity and usually involves realigning or partial removal of bone. It should also be noted that flexible deformities can develop into more rigid deformities.
Hammertoes tend not to resolve by themselves and unfortunately they tend to worsen with time. Surgical correction is done on an out-patient basis, usually utilizing local anesthesia with sedation. Most surgeries allow you to walk-in and walk-out of the surgery facility on the same day. Orthotics and/or good arch supportive shoes may be discussed and encouraged after surgery to lessen the chance of re-occurrence. Prior to any surgery, your doctor will thoroughly discuss the proposed correction and the appropriate after-care.
BUNIONS
That bump on the base of your big toe has gotten larger and become painful. The big toe is beginning to crowd the other toes. Why? A bunion is caused by an imbalance of the muscles around the big toe's base (the first metatarsal phalangeal joint). As the first metatarsal becomes unstable, the muscles around this joint act to pull the big toe toward the second toe. This action also pushes the first metatarsal bone outward. A bunion deformity is the result.
It is the instability around this joint that results in the pathological process. This joint instability, or hypermobility, may be due to a myriad of factors including but not limited to the following:
- Pronation (tendency for the arch to fall and the foot to roll in)
- Congenital ligamentous laxity (loose joints)
- Hereditary predisposition (look at other family members)
- Deformed bones (old trauma/heredity)
- Nerve damage/paralysis
- Trauma or injury to the soft tissues around the joint
Treatment
Treatment for bunions and bunion pain has much to do with relieving pressure over the bunion. Surgical correction also should try to realign the joint to prevent further damage. Treatment is based on accommodation or correction.
Accommodation
Conservative care is almost always an option. This is based primarily on modifying footwear to alleviate pressure. Wider shoes with more toe box room are very helpful. We also recommend using a shoe cobbler to stretch the area over the bunion prominence. The bunion is a sign of an imbalance within the foot. We may also consider using a custom insert to help control foot mechanics and balance the hypermobile first metatarsal. In severe situations with patients who are not operative candidates, we will prescribe custom extra-depth shoes with inserts.
Correction
Surgical correction is another option that many people choose. We recommend that some form of conservative care be attempted prior to surgical intervention. Considerations prior to surgery are many. These include the patient's age, health, lifestyle/activities, expectations, and other foot problems. Surgical procedures are designed to decrease pain, provide stability, and allow a return to function. There are many different types of procedures to meet the needs of many different degrees of deformity.
Surgical Risks
There are risks with almost everything we do. This includes surgery. Surgical correction of bunions has all the risks of any other type of surgery including wound healing, infection, scarring, and discomfort as well as the chance of recurrence. Some of the procedures require cutting and repositioning of the bones that make up the deformity. This requires bone healing. These procedures often use surgical pins or screws to hold position while the bone heals (these may require future removal). Surgery is not a panacea, choose you surgeon carefully.
Almost all bunion procedures are performed in an outpatient setting (hospital or outpatient surgical facility). They are frequently performed under IV sedation, which gives the best and safest results. The patient is asleep throughout the procedure and awakens in the recovery room. Postoperative Plans
What should you expect if you have bunion surgery? Inconvenience?… certainly, and some pain. When I visit my patients after the surgery and healing is over they usually relate two surprises: Minimal pain and real inconvenience. Foot surgery makes getting around quite difficult. The first 4-5 days after surgery should entail rest with foot elevation and bathroom privileges only. This is the most crucial time in the post-operative period. Some procedures require the use of a stiff soled post-operative shoe for 4 weeks followed by a sports shoe for another 4 weeks. Other procedures require a type of cast and non-weightbearing using crutches for a period of 4-6 weeks.
The short term inconvenience and discomfort are lessened by carefully following the post-operative instructions. It is also very important to have excellent communication after surgery. Concerns and worries should be vocalized so that they may be addressed.
NEUROPATHY
Individuals may have symptoms of “pins and needles” in their feet. This sensation is called paresthesia. Others may complain of numbness in all or part of one or both feet. These abnormal sensations, due to general systemic disease or local disorders affecting the nerves, are referred to as neuropathies. Not infrequently, when the cause is a systemic disease, neuropathy is accompanied by deep, painful sores, or ulcers, especially in areas of the foot subject to weight bearing or friction. Painless ulcers are referred to as neuropathic ulcers and are associated with neuropathy. Sometimes the patient has an associated problem that blocks the small or large arteries supplying the skin. This will reduce circulation and nutrition to the skin, making ulceration a greater risk.
Perhaps the most common systemic disease causing neuropathy in the foot is diabetes mellitus, a condition whereby the body either lacks or is unable to properly utilize insulin. Insulin is a chemical made by the body within the cells of the pancreas, a gland found in the abdomen behind the stomach and near the small intestine. Other conditions that cause neuropathies include alcoholism (due to the deficiency in one of the B vitamins called thiamine) and the advanced, or tertiary, stage of syphilis.
Entrapment neuropathy in the foot is caused by some form of compression in an area of the foot referred to as the tarsal tunnel syndrome. It involves a part of the tibial nerve, creating paresthesia and pain in the foot. The tibial nerve lies behind and deep to the inner ankle, and is prone is injury from trauma or foot deformities.
If you think you have neuropathy or have any questions, please make an appointment with our office. We will be glad to meet with you, perform a thorough examination of your feet, and discuss their findings and treatment options with you.
Wound Care
A wound is an opening in the skin. Over one million wounds requiring medical care occur annually. In fact, approximately six million Americans suffer from chronic wounds caused by trauma, surgery, diabetes, arterial and venous disease, edema or pressure. Many of these wounds are on the legs and feet. Generally, wounds heal within eight weeks; however, healing may be delayed if you have circulation problems, diabetes, a collagen disease, history of radiation, or an autoimmune disease. If you have a wound and it is slow to heal, it would be beneficial to talk with Dr. Zimmerman about your problem.
Dr. Zimmerman has advanced training in wound management. As a member of THE AMERICAN PROFESSIONAL WOUND CARE ASSOCIATE, he attends numerous seminars on current wound care techniques. He also is on staff at the Saint Anthony Wound Care Clinic in Chicago.
Our office specializes in the care of these wounds. Our goal is to work together with the patient, family, and other medial providers, focusing on the needs of each individual patient. For chronic wound sufferers, the healing process can be long and frustrating.
A work-up in our office would include a thorough diagnostic evaluation to identify the type of wound and underlying causes. An individually tailored treatment plan is then developed.
Our office will strive not only for excellence of care, but excellence in education. The staff will provide you with the necessary information to help in the healing process.
TAKE GOOD CARE OF YOUR SKIN
- Inspect your skin every day. Use a mirror to look at hard to see areas.
- Look for areas that stay red after a change of position, especially over bony areas: lower back, hips, heels, back of the head, rims of the ears, ankles, elbows, shoulder blades, and spine and for areas that are dry, cracked, bruised, or blistered.
- Keep your skin clean and free from perspiration, urine, stool, and wound drainage.
- Bathe regularly in warm (not hot) water with a mild, pH-balanced product (Dove, Oil of Olay with Shea Butter, Aveeno, Neutrogena). Pat your skin dry in all skin folds and creases. Pay special attention to the area between, under, and around your toes.
- Moisturize your skin at least daily. Do not apply lotions or creams between your toes; only to the tops and bottoms of your feet.





